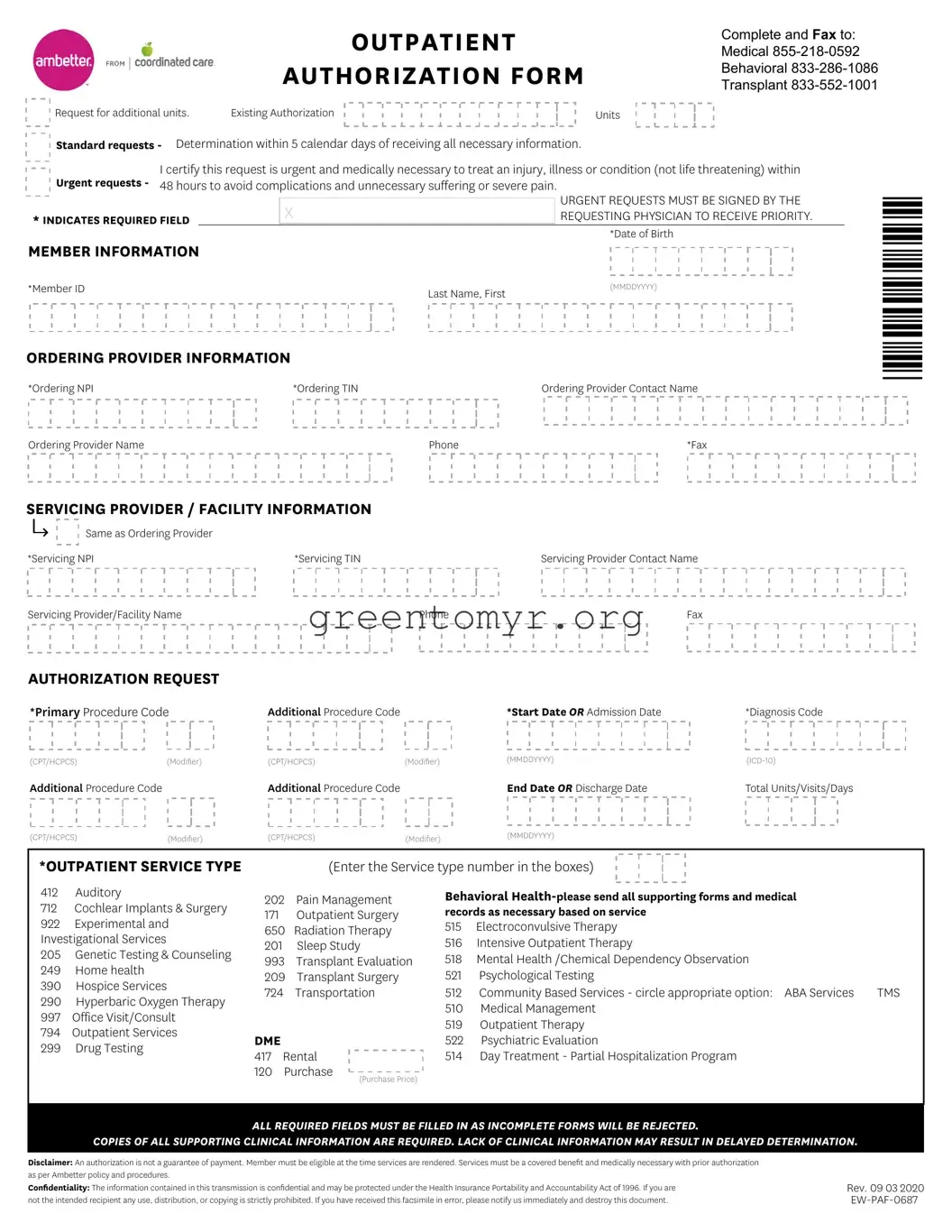
Correctly completing the Ambetter Out Patient form is crucial for efficient processing of medical requests. Many people encounter issues that can lead to delays or even rejections of their submissions. Here are eight common mistakes to avoid when filling out the form.
First, many individuals overlook the required fields. Every section marked with an asterisk (*) must be filled out. Omitting even one of these fields can result in the entire form being deemed incomplete, leading to rejection. Careful attention to these details will help facilitate a smoother authorization process.
Another frequent error is incorrectly entering the member’s information. The Member ID, last name, and first name should be accurately entered as they appear on the member’s insurance card. Double-checking these entries ensures that the request is easily matched with the member's file.
People often neglect to provide complete ordering provider information. This includes the Ordering NPI (National Provider Identifier) and TIN (Tax Identification Number) along with the provider's name and contact details. Incomplete information can create hurdles in verifying the provider's credentials, delaying authorization.
In many instances, individuals select the incorrect service type on the form. Each service type has a specific code that allows for proper categorization of the request. Ensuring that the correct service type number is entered guarantees that the request is processed under the right guidelines.
Another mistake made is not specifying the diagnosis code properly. The form requires accurate ICD-10 codes to substantiate the medical necessity of the requested services. Inaccurate codes can lead to misunderstandings about the patient’s condition and can impede approval.
Some individuals fail to include the necessary supporting documentation. The form clearly states that copies of all clinical information are mandatory. Without these, the request may experience significant delays, as the review team cannot make an informed decision about the authorization.
Moreover, people sometimes do not check if the services are a covered benefit under the member’s plan. Familiarizing oneself with the coverage details can prevent surprises down the line, ensuring that the requested services align with their insurance policy.
Finally, many individuals overlook the importance of signing the form when submitting urgent requests. An unsigned urgent request will not be processed, even if it clearly indicates a need for rapid response. This oversight can result in unnecessary delays in patient care.
By being aware of these common pitfalls and taking the time to fill out the Ambetter Out Patient form carefully, individuals can improve their chances of timely and efficient authorization for medical services.