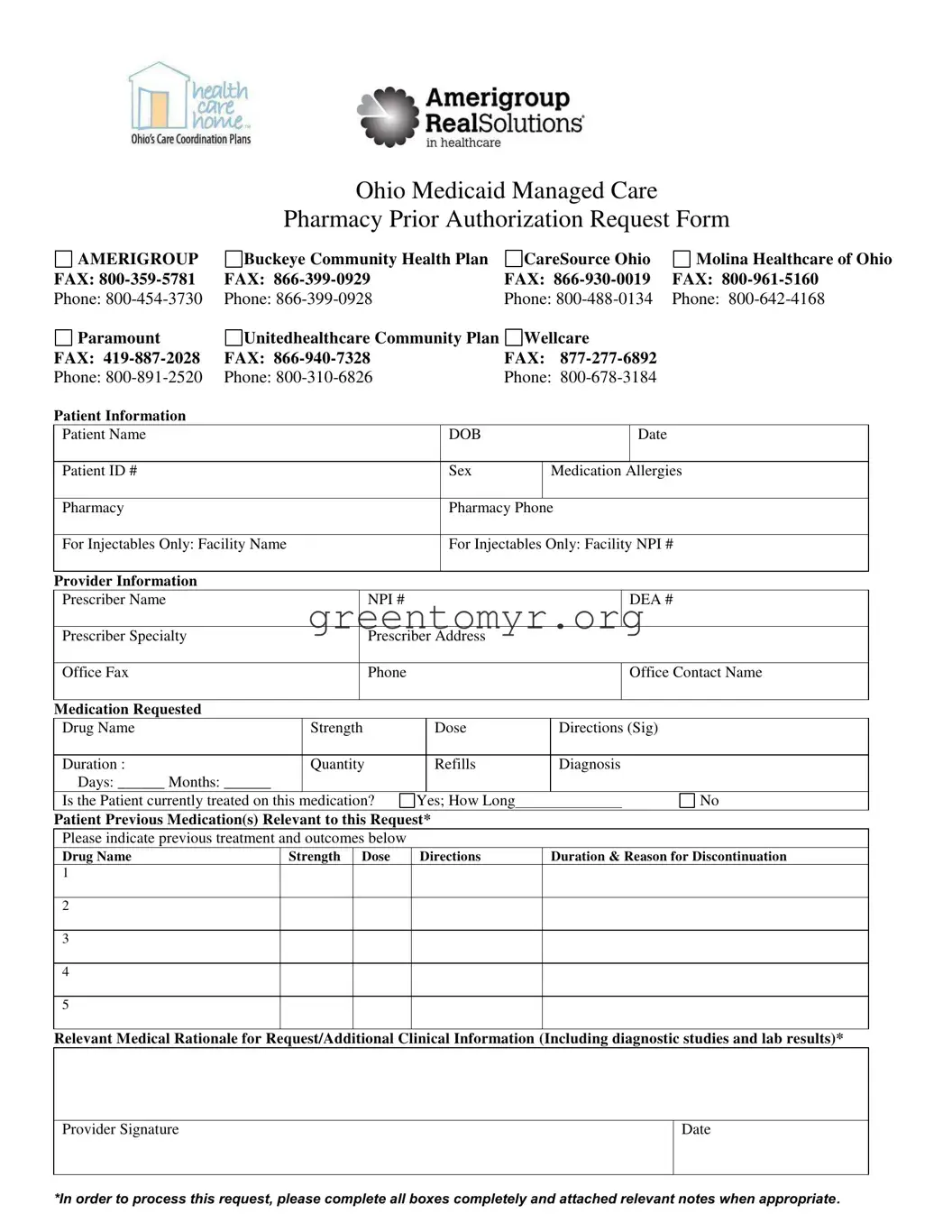
When filling out the Amerigroup Authorization Request form, it is crucial to avoid common mistakes that can delay the approval process. One significant error is leaving the patient information section incomplete. This section requires details such as the patient’s name, date of birth, and ID number. If any of this information is missing, the request may be rejected or cause unnecessary delays.
Another frequent mistake involves failing to include relevant medical rationale for the medication request. Inadequate clinical justification may lead to a denial of the authorization. Documentation of diagnostic studies and lab results should be provided to support the need for the requested medication.
Inaccuracies in the medication requested section can also hinder the process. It is imperative to ensure the drug name, strength, and dosing directions are correct. Any discrepancies could raise questions and result in a delay while the information is verified.
Some individuals neglect to indicate previous medications related to the request. If the form asks to list previous treatments and their outcomes, it is essential to answer this thoroughly. Without this context, the need for the new medication may not be clear, which could lead to an outright denial.
Additionally, omitting the provider’s information can be problematic. It's essential to include the prescriber’s name, NPI number, and contact details. This enables the review team to reach out for any clarifications without unnecessary back-and-forth communication.
A common oversight is not providing a complete duration and quantity for the medication requested. Clearly specifying these details helps in assessing the request's appropriateness and aligns with standard health practices.
Failing to sign and date the form can also lead to processing issues. The provider's signature is a legal affirmation of the information provided and is essential to complete the authorization request.
Lastly, submitting the form without relevant notes or attachments when necessary can result in a lack of crucial context. Always attach any pertinent documents that could support the request, such as previous treatment plans or lab results. This additional information can significantly aid in the decision-making process.