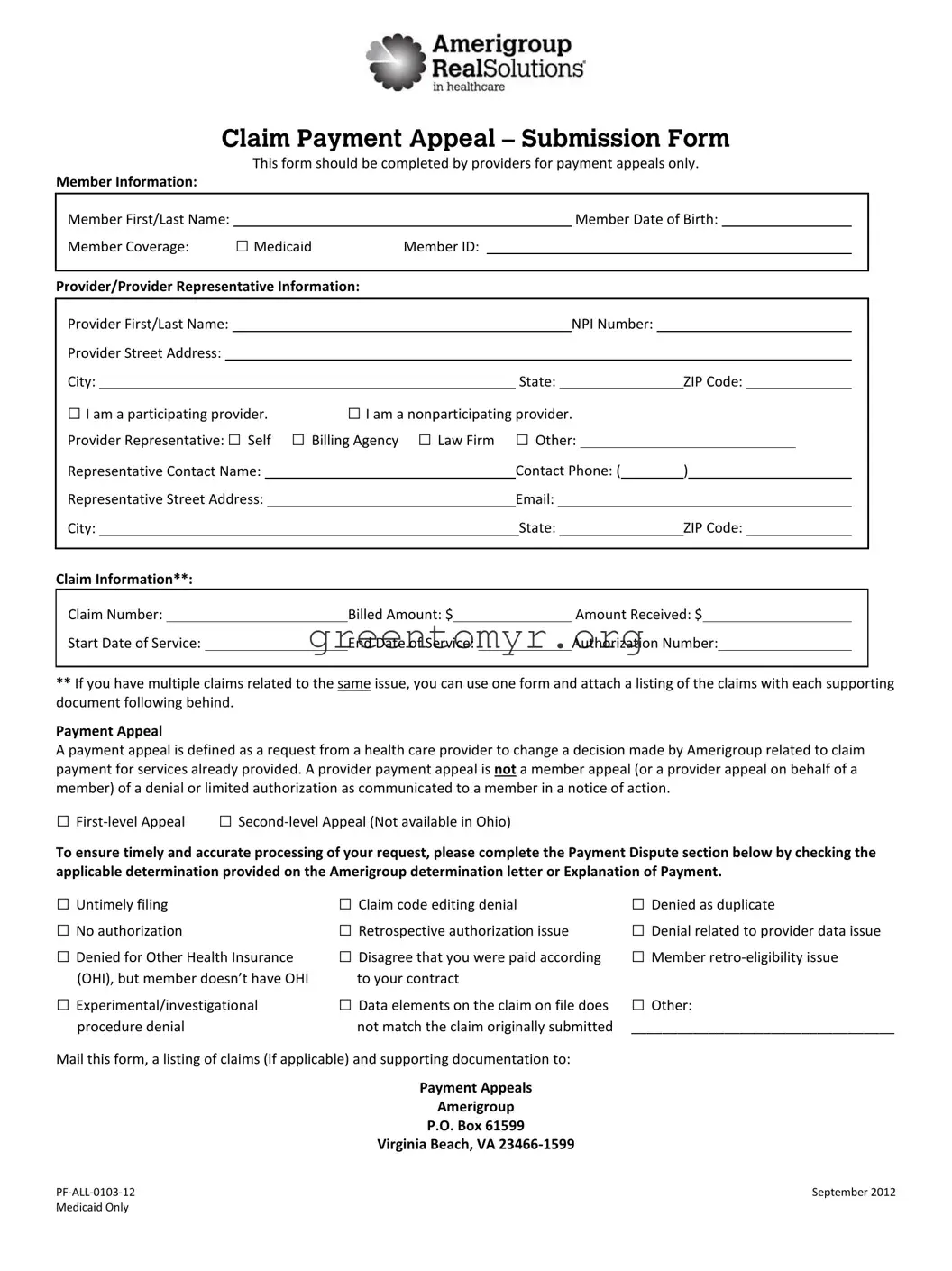
The Amerigroup Medicaid Claim Payment Appeal Submission Form serves as a crucial tool for healthcare providers seeking to contest decisions made regarding claim payments for services rendered. This form is specifically designed for payment appeals, allowing providers to collect and submit pertinent information related to a member's coverage. Essential details to include are the member's first and last name, date of birth, and Medicaid Member ID, which help to verify eligibility and identify the specific case. Additionally, the form requires the provider’s information, such as the name, NPI number, and address, as well as the representative's contact information if applicable. Important claim details, including the claim number, billed amount, amount received, dates of service, and authorization number, must also be clearly outlined. Healthcare providers can utilize this form for both first-level and second-level appeals, detailing the specific grounds for payment disputes, such as untimely filing, duplicate claims, or lack of authorization. To ensure a thorough and efficient review process, one may attach a list of related claims and necessary supporting documents, which can help expedite the resolution of the appeal. Once completed, the form should be sent to the designated address provided by Amerigroup to initiate the appeal process.