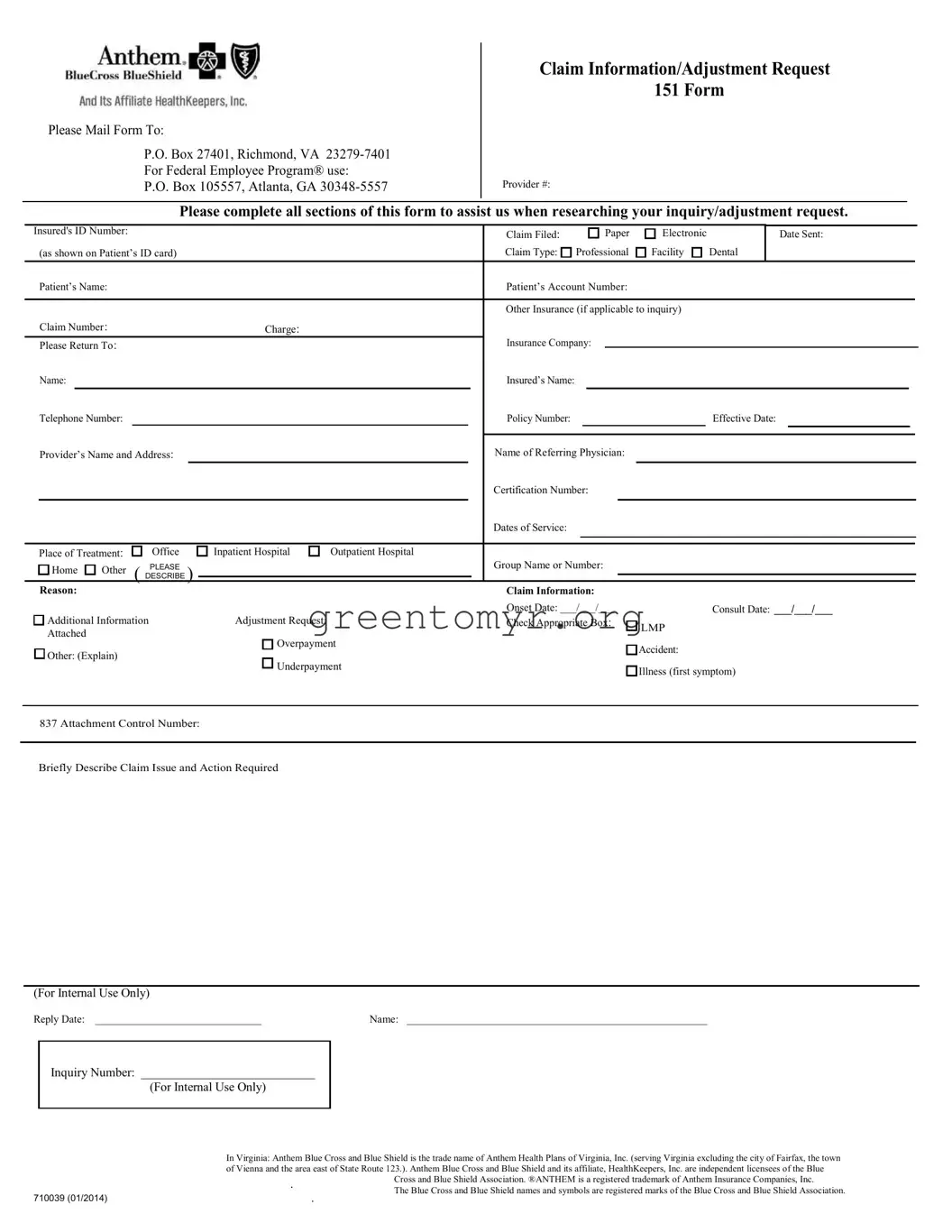
Filling out the Anthem 151 form can be straightforward, but people often make mistakes that may delay processing. One common error is leaving sections incomplete. Each section of the form needs to be filled out to ensure that the claim is handled efficiently. Skipping even a single part can lead to unnecessary back-and-forth communication.
Another mistake occurs when incorrect identification numbers are provided. It's important to double-check the Insured's ID Number and Claim Number for accuracy. Misstating these numbers can result in significant delays as the claim may need to be resubmitted with the right information.
Some individuals forget to indicate whether the claim was filed on paper or electronically. This detail helps Anthem streamline the process. Including this information can prevent confusion and speed up the inquiry.
People also tend to overlook specifying the Claim Type. The form includes options like Professional, Facility, or Dental. Selecting the correct type is crucial for directing the claim to the right department and getting an appropriate response.
Another issue is failing to provide the Reason for the inquiry or adjustment request. Clearly stating the reason allows Anthem to understand the situation better. Vague explanations may lead to additional questions and possible delays.
Along with this, some forget to attach necessary documents, such as overpayment or adjustment request details. Supporting documents are essential for clarity and can expedite the review process. Reviewers depend on these attachments to assess the claim correctly.
Additionally, people might mistakenly use outdated or incorrect addresses when sending the form back. It is always advisable to confirm that the mailing address is current. Using the wrong address can prevent timely processing.
Misunderstanding the requirement for the Dates of Service is another frequent oversight. Clearly listing these dates can help identify the timeline of the claim and avoid further confusion. Ensure these dates align with the medical services provided.
Finally, some individuals neglect to include a brief description of the claim issue. This description is helpful for internal processing and can clarify the request. A well-articulated summary aids in a quicker resolution.

 LMP
LMP