Filling out the Arizona Do Not Resuscitate Order form can be a crucial step for individuals planning for their healthcare preferences. However, many make common mistakes that can lead to confusion or complications. It's important to avoid these errors to ensure your wishes are clearly communicated.
One frequent mistake is failing to include the date when the form is signed. This date establishes when the directives become effective. Without it, medical professionals may question the validity of the order or its timeline.
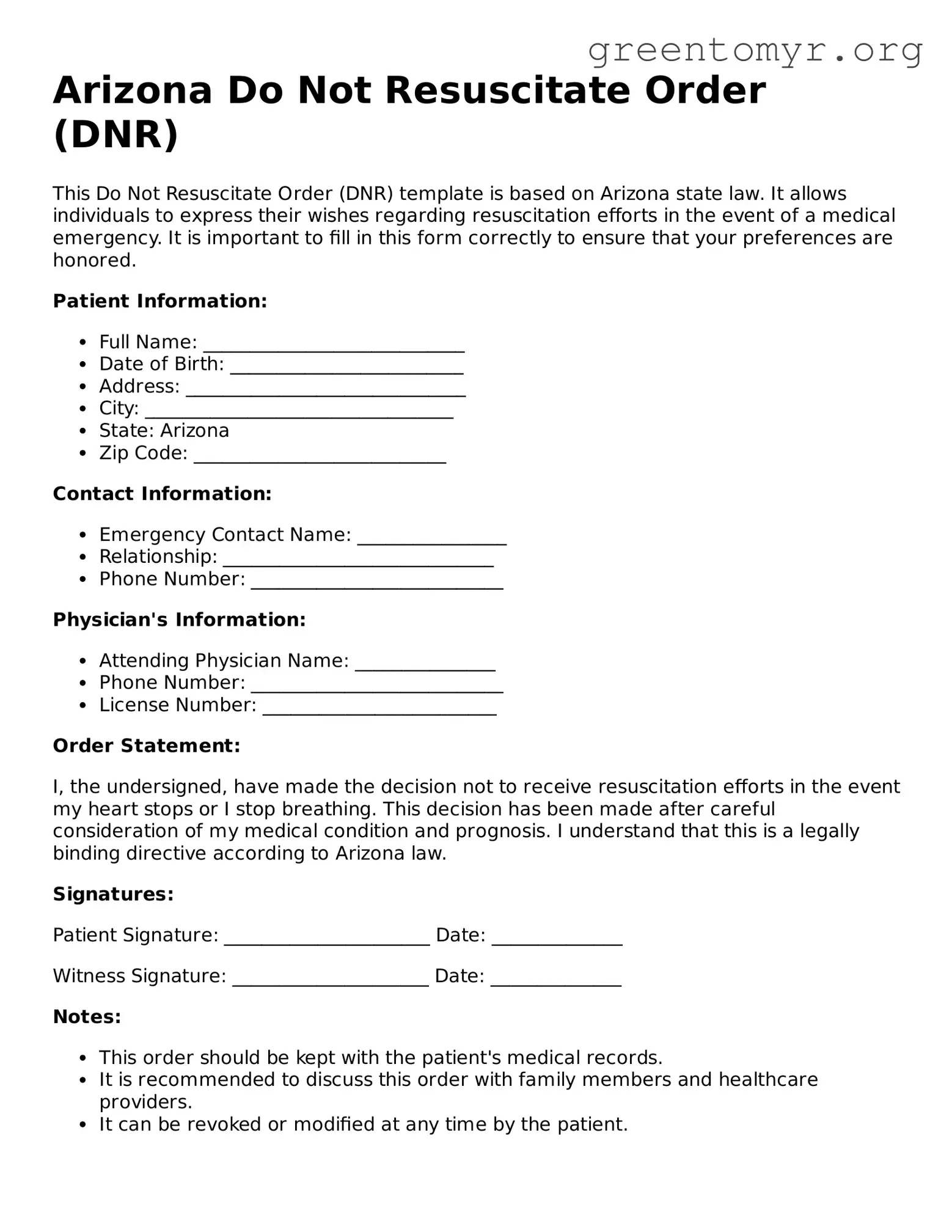
An incomplete or incorrect signature can render the form void. Ensure that all required parties, including a witness if necessary, sign the document where indicated. Double-check to confirm that signatures are legible and do not contain errors. Missing a signature creates delays when attempting to enforce your wishes.
Another common pitfall is using an outdated form. Arizona law occasionally updates these documents. Always verify that you are using the most recent version of the Do Not Resuscitate Order form to avoid issues with acceptance by healthcare providers.
People also often forget to make copies of their completed forms. Keeping a copy on hand allows you to provide it easily to healthcare providers when needed. Additionally, share copies with family members or close friends to ensure they are aware of your wishes.
Inaccurate patient information is another major error. Verify that all personal information, such as your name, address, and date of birth, is correct. Typos or inaccuracies can lead to misunderstandings during a medical emergency.
Many individuals neglect to discuss their decisions with family members. Open conversations about your Do Not Resuscitate Order help ensure that your loved ones understand and support your choices. Without this conversation, misunderstandings may arise during critical moments.
Finally, some people mistakenly believe the process ends once they submit the form. Regularly review your Do Not Resuscitate Order, especially after major life changes such as health status or family dynamics. Keeping your documents up-to-date ensures they accurately reflect your current wishes.