AUTHORIZATION FOR SPECIAL SERVICES IS NOT REQUIRED IN AN EMERGENCY
1.This form is used for a workers' compensation, volunteer firefighters' or volunteer ambulance workers' benefit case to request written authorization for special service(s) costing over $1,000 in a non-emergency situation or requiring pre-authorization pursuant to the Medical Treatment Guidelines.
2.This form must be signed by the attending doctor and must contain her/his authorization number and code letters. Out-of-State medical providers must enter their NPI number. If the patient is hospitalized, it may be signed by a licensed doctor to whom the treatment of the case has been assigned as a member of the attending staff of the hospital.
3.Please ask your patient for his/her WCB case # and the claim administrator claim (carrier case) number and show these numbers on this form. In addition, ask your patient if he/she has retained a representative. If represented, ask for the name and address of the representative.
This request must be sent to the Workers' Compensation Board, and the the workers' compensation insurance carrier, self-insured employer, or Special Fund. If patient is not represented, a copy must be sent to the patient.
4.The attending doctor must submit this form with the Board and on the same day serve a copy on the self-insured employer or the insurer by one of the following methods of service: a) the insurer's designated fax number, b) the insurer's designated email address, or c) by regular mail with confirmation of delivery. The insurer's designated fax and email address can be found at: wcb.ny.gov/attending-doctors-request-authorization. Failure to submit the request to the designated contact identified on the WCB's website may result in your request being denied. If there is no designated contact listed on the WCB website, check the "Designated contact information not available" box which is located at the bottom of Section C of this form.
5.If authorization or denial is not forthcoming within 30 calendar days, (or 35 days if C-4AUTH is mailed return receipt requested), the treatment is deemed authorized and the attending physician may provide the requested treatment.
6.SPECIAL SERVICES - Services for which authorization must be requested are as follows:
Physicians - To engage the services of a specialist, consultant, or a surgeon, or to provide for X-ray examinations or physiotherapeutic or other procedures, or to provide for special diagnostic laboratory tests costing more than $1,000.
Podiatrists - In treating the foot, to provide physiotherapeutic procedures, X-ray examinations, or special diagnostic laboratory tests costing more than $1,000. Chiropractors - In treating a condition as provided in Section 6551 of the Education Law, to engage the services of a specialist, consultant, or a surgeon, or to provide for X-ray examinations or physiotherapeutic or other procedures, or to provide for special diagnostic laboratory tests costing more than $1,000.
Occupational/Physical Therapists - In treating a condition as provided in Article 136 or 156 of the Education Law, in the Workers' Compensation Law, and the Rules of the Chair relative to Occupational/Physical Therapy Practice to provide occupational/physical therapy procedures costing more than $1,000.
Psychologists - Prior authorization for procedures enumerated in section 13-a(5) of the Workers' Compensation Law costing more than $1,000 must be requested from the self-insured employer or insurer. In addition, authorization must be requested for any biofeedback treatments, regardless of the cost, or and special diagnostic laboratory tests which may be performed by psychologists. Where a patient has been referred by an authorized physician to a psychologist for evaluation purposes only and not for treatment, prior authorization must be requested if the cost of consultation exceeds $1,000.
Medical Treatment Guidelines - Lumbar Fusions, Artificial Disk Replacement, Vertebroplasty, Kyphoplasty, Electrical Bone Growth Stimulators, Spinal Cord Stimulators, Osteochondral Autograft, Autologus Chondrocyte Implantation, Meniscal Allograft Transplantation, Knee Arthroplasty (total or partial knee joint replacement), Intrathecal Drug Delivery (pain pumps).
7.If the insurer has checked "GRANTED WITHOUT PREJUDICE" in Section C, the liability for this claim has not yet been determined. This authorization is made pending final determination by the Board. Pursuant to 12 NYCRR § 325-1.4(b)(2), this authorization is limited to the question of medical necessity only and is not an admission that the condition for which the services are required is compensable. This authorization does not represent an acceptance of this claim by the insurer, self-insured employer, employer or Special Fund or guarantee payment for the services authorized. When a decision is rendered regarding liability, you will receive a Notice of Decision by mail. The insurer, self-insured employer, employer or Special Fund will only provide payment for these services if the claim is established and the insurer, self-insured employer, employer or Special Fund is found to be responsible for the claim.
8.It is the attending doctor's burden to set forth the medical necessity of the special services required. Be sure to provide this information in the Statement of Medical Necessity section of this form.
9.HIPAA NOTICE - In order to adjudicate a workers' compensation claim, WCL13-a(4)(a) and 12 NYCRR 325-1.3 require health care providers to regularly file medical reports of treatment with the Board and the insurer or employer. Pursuant to 45 CFR 164.512 these legally required medical reports are exempt from HIPAA's restrictions on disclosure of health information.
ANY PERSON WHO KNOWINGLY AND WITH INTENT TO DEFRAUD PRESENTS, CAUSES TO BE PRESENTED, OR PREPARES WITH KNOWLEDGE OR BELIEF THAT IT WILL BE PRESENTED TO OR BY AN INSURER, OR SELF-INSURER, ANY INFORMATION CONTAINING ANY FALSE MATERIAL STATEMENT OR CONCEALS ANY MATERIAL FACT SHALL BE GUILTY OF A CRIME AND SUBJECT TO SUBSTANTIAL FINES AND IMPRISONMENT.
This form must be served on the insurer/self-insurer's designated contact identified on the Board's website:
www.wcb.ny.gov by fax, email or mailed, return receipt requested. Failure to submit the form to the designated contact identified on the Board's website may result in your request being denied. A copy of the form must also be filed with the Board.
NYS Workers' Compensation Board
PO Box 5205
Binghamton, NY 13902-5205
Email Filing: [email protected] l |
Customer Service: (877) 632-4996 l Statewide Fax: (877) 533-0337 |
C-4AUTH (9-19) |
THE WORKERS' COMPENSATION BOARD EMPLOYS AND SERVES PEOPLE WITH DISABILITIES WITHOUT DISCRIMINATION |

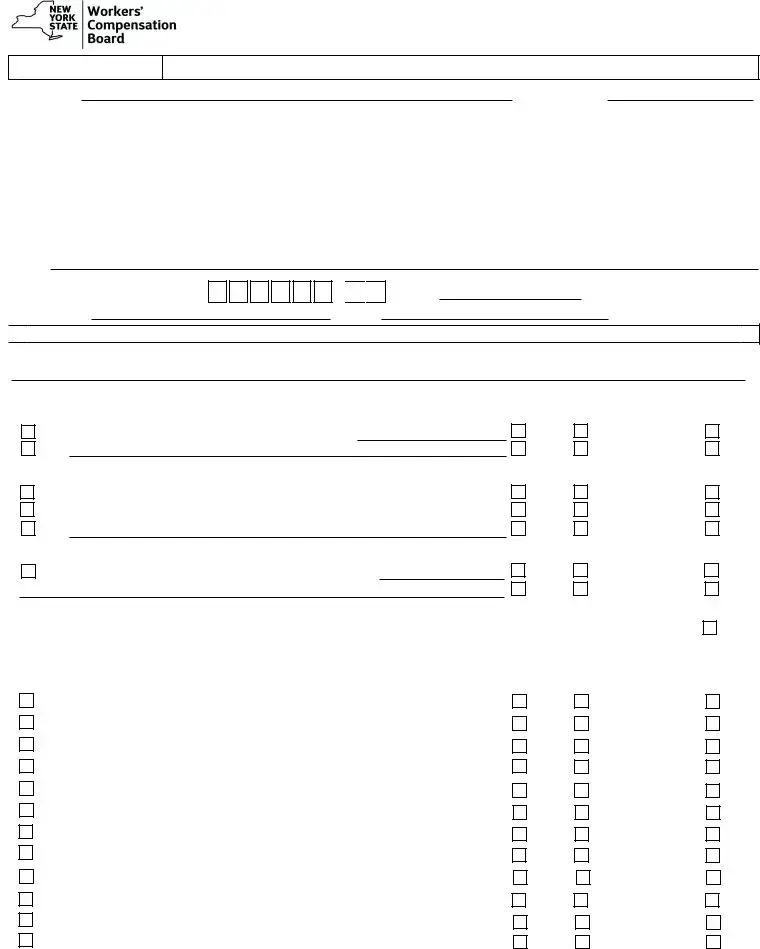



 AUTHORIZATION REQUEST
AUTHORIZATION REQUEST