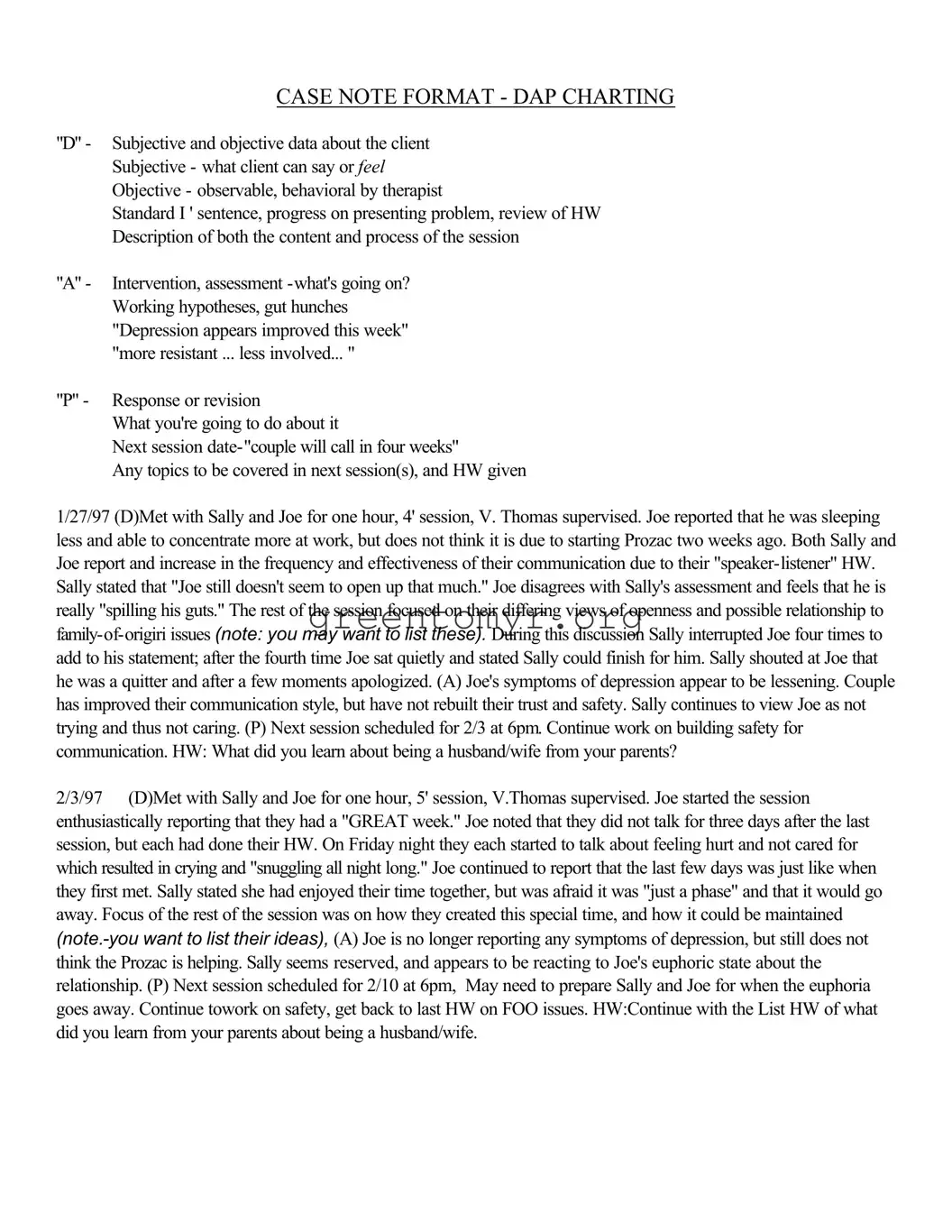
CASE NOTE FORMAT - DAP CHARTING
"D" - Subjective and objective data about the client Subjective - what client can say or FEEL Objective - observable, behavioral by therapist
Standard I ' sentence, progress on presenting problem, review of HW Description of both the content and process of the session
"A" - Intervention, assessment -what's going on? Working hypotheses, gut hunches "Depression appears improved this week" "more resistant ... less involved... "
"P" - Response or revision
What you're going to do about it
Next session date-"couple will call in four weeks"
Any topics to be covered in next session(s), and HW given
1/27/97 (D)Met with Sally and Joe for one hour, 4' session, V. Thomas supervised. Joe reported that he was sleeping less and able to concentrate more at work, but does not think it is due to starting Prozac two weeks ago. Both Sally and Joe report and increase in the frequency and effectiveness of their communication due to their "speaker-listener" HW. Sally stated that "Joe still doesn't seem to open up that much." Joe disagrees with Sally's assessment and feels that he is really "spilling his guts." The rest of the session focused on their differing views of openness and possible relationship to family-of-origiri issues (note: you may want to list these). During this discussion Sally interrupted Joe four times to add to his statement; after the fourth time Joe sat quietly and stated Sally could finish for him. Sally shouted at Joe that he was a quitter and after a few moments apologized. (A) Joe's symptoms of depression appear to be lessening. Couple has improved their communication style, but have not rebuilt their trust and safety. Sally continues to view Joe as not trying and thus not caring. (P) Next session scheduled for 2/3 at 6pm. Continue work on building safety for communication. HW: What did you learn about being a husband/wife from your parents?
2/3/97 (D)Met with Sally and Joe for one hour, 5' session, V.Thomas supervised. Joe started the session enthusiastically reporting that they had a "GREAT week." Joe noted that they did not talk for three days after the last session, but each had done their HW. On Friday night they each started to talk about feeling hurt and not cared for which resulted in crying and "snuggling all night long." Joe continued to report that the last few days was just like when they first met. Sally stated she had enjoyed their time together, but was afraid it was "just a phase" and that it would go away. Focus of the rest of the session was on how they created this special time, and how it could be maintained (note.-you want to list their ideas), (A) Joe is no longer reporting any symptoms of depression, but still does not think the Prozac is helping. Sally seems reserved, and appears to be reacting to Joe's euphoric state about the relationship. (P) Next session scheduled for 2/10 at 6pm, May need to prepare Sally and Joe for when the euphoria goes away. Continue towork on safety, get back to last HW on FOO issues. HW:Continue with the List HW of what did you learn from your parents about being a husband/wife.
|
Writing Behavioral Goals |
Lends itself to any 2 people agreeing the goal is met |
Subject + verb |
-Client will/will not |
Action |
-Be able to sleep |
Frequency |
-At least five nights per week |
Duration |
-For three consecutive weeks |
Monitor |
-As observed by husband |
Goals:
·Measurable
·Observable
·Time-limited
·Target-dated
·Realistic (achievable)
·Relevant (to the problem)
·Appropriate
·Consistent with the client's values
·Should be able to describe what the client should be able to do to demonstrate improvement/symptom relief
Everything You Ever Wanted To Know About Case Notes
·Think about what you are going to write and formulate before you begin
·Be sure you have the right chart!
·Date and sign every entry
·Proofread
·Record as "late entry" anytime it doesn't fall in chronological order; be timely
·Think about how the client comes through on paper
·Watch abbreviations-use only those approved
·Errors should have a line through incorrect information. Write error,intital and date
·Write neatly and legibly; print if handwriting is difficult to read
·Use proper spelling, grammar and sentence structure
·Don't leave blank spaces between entries; can imply vital information left out
·Put client name/case number on each page
·Avoid slang,curse words
·Another provider should be able to continue quality care
·Use quotes from client that are clinically pertinent Use descriptive terms
·Describe what you observed, not just your opinion of what you observed
·Reference identified problems from the treatment plan
·Reference diagnostic criteria from DSM-lV
·Use power quotes:
"Client remains at risk for _____________ as evidenced by ___________”
"The current symptoms include _____________”
"Limited progress in ___________”
"Continues to be depressed as evidenced by ____________”
"Client continues to have suicidal ideation as evidenced by the following comment made
to this writer: ____________”
Who Relies On Your Documentation?
Clients’ Families
Rely on your documentation to advocate for the most appropriate and effective care
Physicians
Mental Health Professionals
Referral Sources
Rely on the medical record as an official and practical means of communicating with each other
Rely on your documentation to help them provide a unified treatment approach consistent with your work with the client
Rely on your documentation to provide continuity of care from one treatment setting to another
Employers
Other Payors
Managed Care Companies
Rely on your documentation to justify need for continued treatment, need for admission, demonstrate appropriateness and cost-effectiveness of care, demonstrate all billable services were provided
Licensing and Accreditation Agencies
Rely on your documentation to verify your practice's quality of care and approve your license to operate
Chart Order
Left side
·Case Contact Summary Sheet
·Intake Form
·Client Information Questionnaire
·Release of Information Cover Letter
·Release of Information from Purdue Marriage and Family Therapy Center
·Informed Consent for Treatment
·Fee Contract
·Fee Receipts (balanced)
·Quality Assurance Review Sheets
Right side
·Treatment Plan (formulated by the 3rd session)
·Case Notes
·All drawings, correspondence, and other direct therapy documentation
·Termination/Transfer/Unopened Case Summaries