Filling out a Do Not Resuscitate (DNR) Order form is an important decision that reflects one's wishes about medical treatment in the event of a critical health situation. However, many individuals make mistakes during this process that can lead to confusion or unintended consequences. Recognizing these common pitfalls can help ensure that the form accurately represents the individual's intent.
One significant mistake occurs when people don't communicate their decisions clearly to family members. Even if the DNR form is completed correctly, if loved ones are unaware of its existence or the reasons behind the decision, this can lead to misunderstandings and distress during medical emergencies. It’s essential to have open discussions about this choice and ensure that family members know where the form is located.
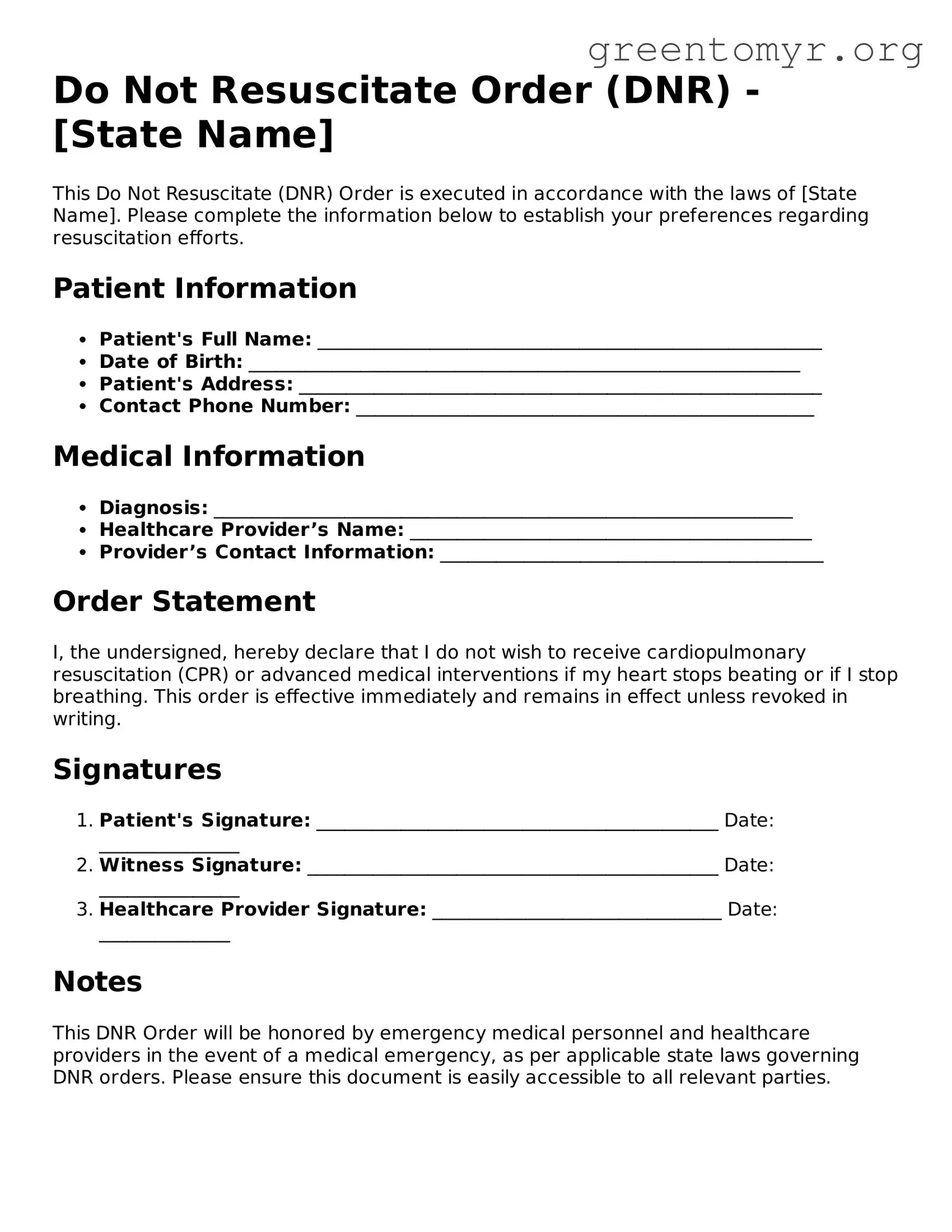
Another frequent error is using outdated or incorrect forms. Medical protocols and legal requirements may change over time. Individuals should ensure they are using the most recent version of the DNR Order form specific to their state or healthcare provider. Filling out an obsolete form can render the document invalid, leading to confusion at critical moments.
People often forget to specify the level of care they wish to receive before the point of resuscitation. A DNR does not imply a desire for no medical intervention. It’s crucial to clarify what types of treatment are desired prior to a resuscitation attempt. Patients should consider discussing their wishes with a healthcare professional to highlight the nuances of their choices.
Failing to sign and date the form is another common mistake. A DNR Order must be signed by the patient or their designated representative. Additionally, most states require the signature of a witness or a healthcare provider. Forms that lack proper signatures may not be honored by medical personnel. Always double-check that all necessary sections are completed.
Many individuals misunderstand who can act as a healthcare proxy. Designating a healthcare proxy on the DNR form is an important aspect. Sometimes, people assume that just anyone can serve in this role. In reality, it is vital to choose someone who understands your wishes and is prepared to advocate on your behalf, should the need arise.
Another mistake is not storing the DNR Order in an accessible location. The form should be placed in a visible and easily reachable spot, such as on the refrigerator or in a file with other important documents. When emergencies occur, medical professionals need to locate the DNR quickly, and hiding the form could result in unwanted interventions.
People often overlook the need to review and update their DNR Orders periodically. Life circumstances change, and so may a person's preferences regarding medical care. Regularly checking the form ensures that it still accurately reflects current wishes and allows for adjustments based on changes in health or personal philosophy.
Lastly, individuals sometimes neglect to inform healthcare providers of their DNR status. If a DNR Order exists but has not been communicated to the relevant medical personnel, it could lead to unwanted resuscitation efforts. Patients should provide copies of the order to their primary care physician and other healthcare facilities to create an open line of communication.
By being mindful of these common mistakes when completing a DNR Order form, individuals can help ensure that their wishes are respected and honored. Open communication, proper documentation, and regular reviews can make a significant difference in the event of an emergency, providing peace of mind to both the individual and their loved ones.