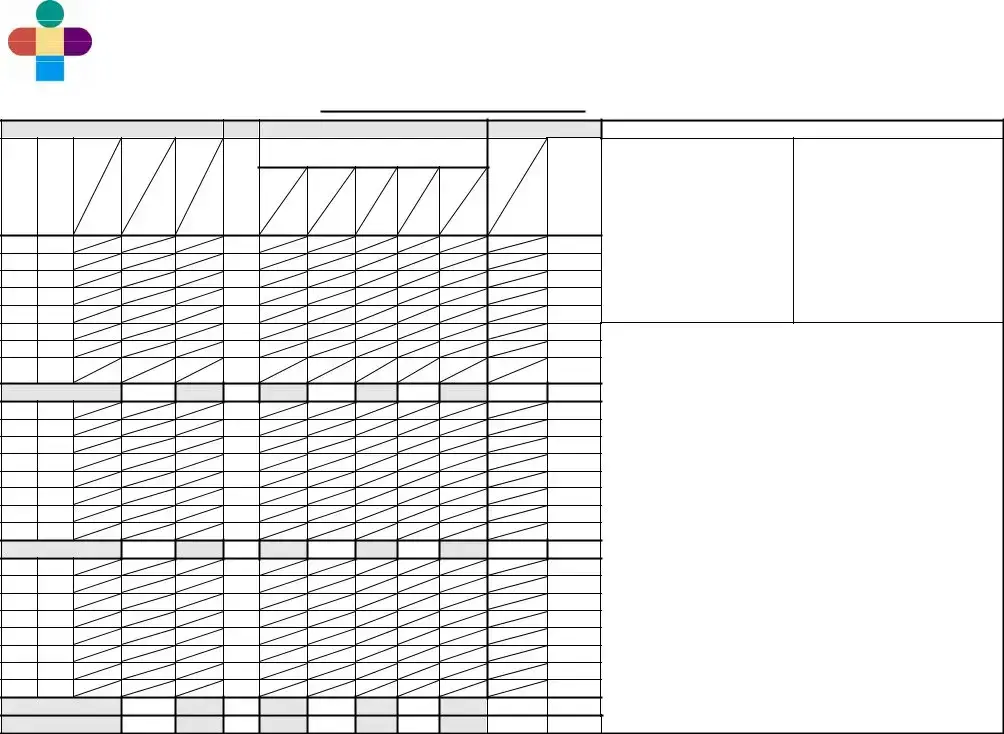
GENERAL
R – Right
L – Left
- Done
-- Absent
+ - Present - Increased - Decreased
‡- Asymmetrical = - Equal
- Changed
BED
I – Isolette
OC – Open Crib
OW – Open Warmer
HR QUALITY
R – Regular
I – Irregular
M – Murmur
RESP. PATTERN
R – Regular
IR – Irregular
S – Shallow
PB – Periodic
Breathing
BP SITE
LA – Left Arm RA – Right Arm
LL– Left Calf RL – Right Calf LT – Left Thigh RT – Right Thigh
BREATH SOUNDS
Cr – Crackles
C – Clear
CO – Coarse
W – Wheeze
S – Stridor
AIR ENTRY
G – Good
L – Limited
T – Tight
EQUALITY
++- Bilaterally RorL - Diminished - Diminished
bilaterally
RETRACTIONS
M – Minimal
MO – Moderate
S – Severe
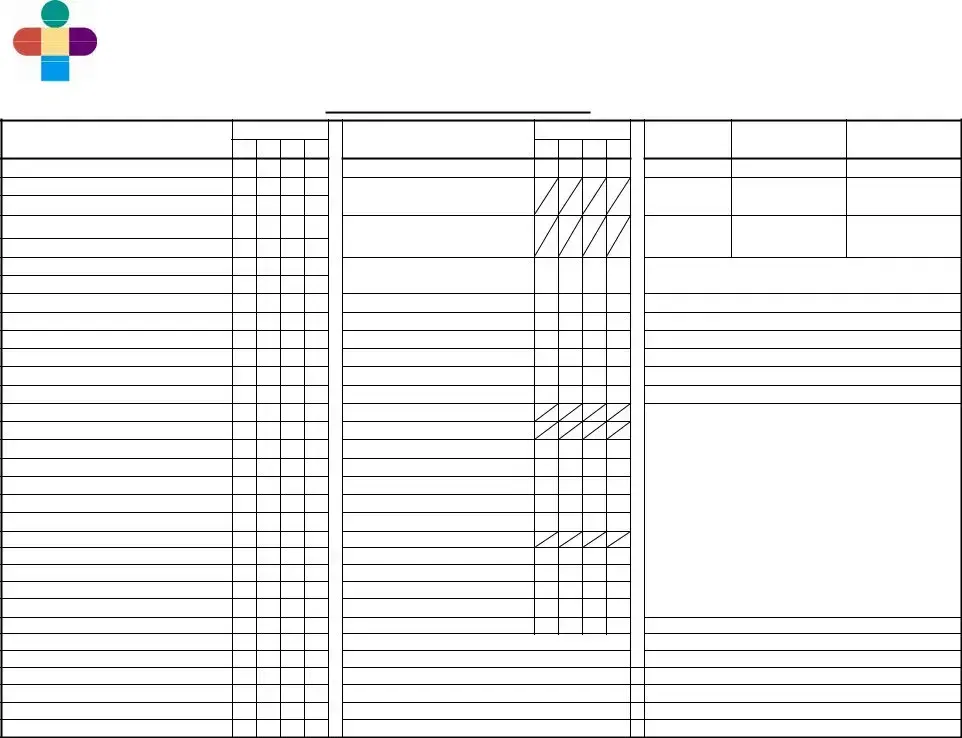
BEHAVIOR DURING BREASTFEEDING
1Latches on without difficulty with strong, steady and rhythmic sucks; briefly pauses and readily resumes sucking; frequent,
coordinated suck- swallowing heard
2Latches on without difficulty with strong, steady and rhythmic sucks; briefly pauses
and resumes sucking without help; some swallowing heard.
3 Latches on with minimum difficulty; sucks are short and quick without steady rhythm; pauses and needs help to resume sucking; occasional swallowing heard.
4Roots or licks; latches on with difficulty; briefly maintains latchon or does not suck;
no swallowing heard.
5 Roots or licks; unable to latch on for breastfeeding attempt.
6No effort (sleepy, lacks energy, has no interest, cries, squirms, or pushes away) despite much assistance, unable to successfully attempt breastfeeding.
RESPONSE TO FEEDING
1Appears satiated and comfortable; becomes relaxed, quietly interactive or sleepy without
physiologic changes.
2Becomes tired and fatigued from feeding; has minimal in HR, resp, color or tone.
3Exhausted or taxed by feeding; has changes in resp, color, loss of tone or other
physiologic signs (hiccups, grunts/sounds, cough/choke, head bobbing, O2 sats)
resulting from efforts to feed.
4Has difficulty settling; appears uncomfortable following feeding (shifting within position, straining, spitting, fussiness and/or increased respiratory effort).
SUPPORTS
OB - Occasional Breaks/Pauses
FB - Frequent Breaks/Pauses
PH - Pacing Help
BU - Frequent Burps
FA -Flow Adjustment
SP - Sidelying Position
OP - Other Position
CS - Chin/Cheek Support
OX - Oxygen
EN - Environment
Other - Specify
TYPE OF NIPPLE |
|
|
Y - Yellow |
SF- Slow Flow |
R - Red |
P - Playtex |
|
N - Nuk |
H - Haeberman |
G – Gerber Premie |
SL=Slit |
|
Eff. 9/1/11 Rev. |
Page 3 of 4 |