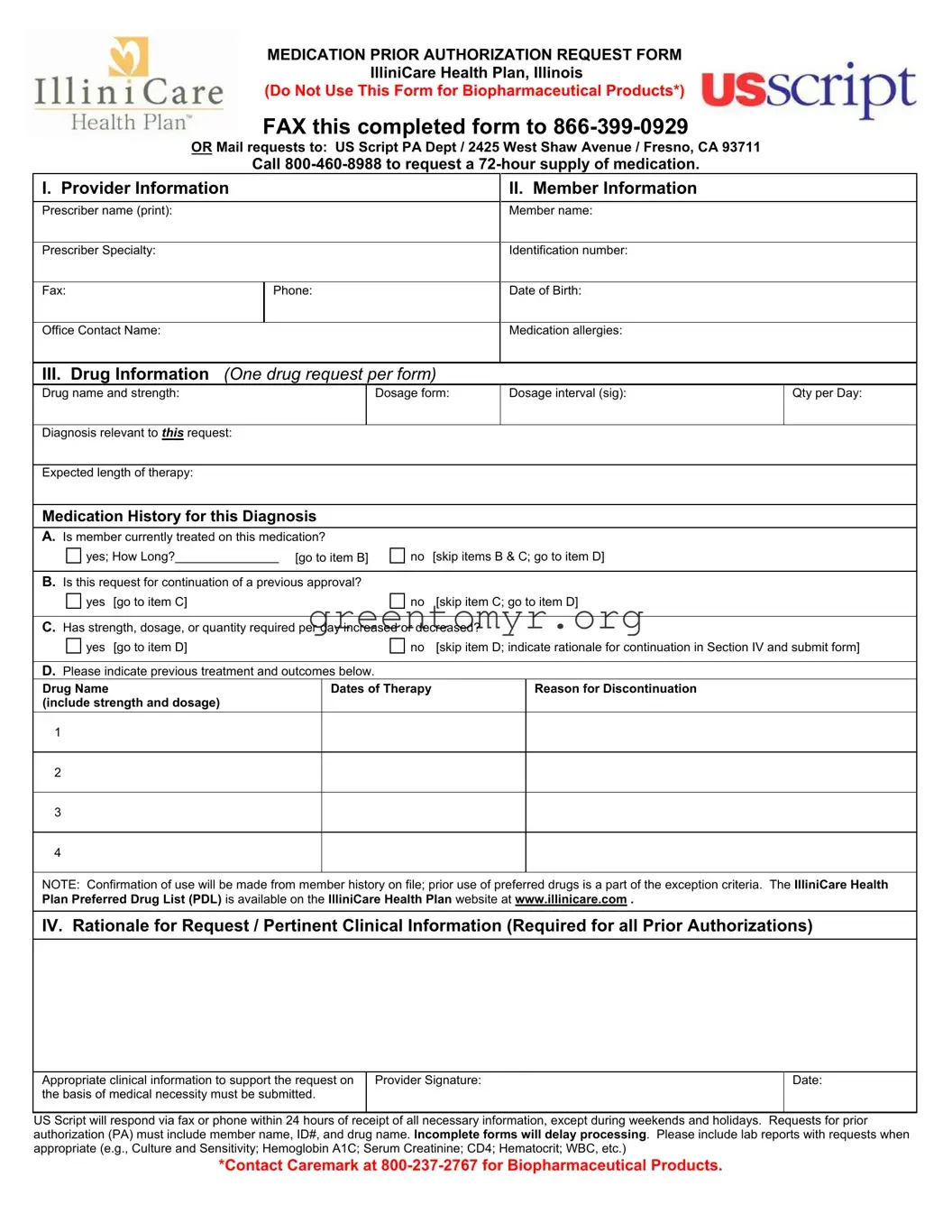
MEDICATION PRIOR AUTHORIZATION REQUEST FORM
IlliniCare Health Plan, Illinois
(Do Not Use This Form for Biopharmaceutical Products*)
FAX this completed form to 866-399-0929
OR Mail requests to: US Script PA Dept / 2425 West Shaw Avenue / Fresno, CA 93711
Call 800-460-8988 to request a 72-hour supply of medication.
I. Provider Information |
|
|
II. Member Information |
|
|
|
|
|
|
|
|
|
|
Prescriber name (print): |
|
|
Member name: |
|
|
|
|
|
|
|
|
|
|
Prescriber Specialty: |
|
|
Identification number: |
|
|
|
|
|
|
|
|
|
|
|
Fax: |
|
Phone: |
|
|
Date of Birth: |
|
|
|
|
|
|
|
|
|
|
Office Contact Name: |
|
|
Medication allergies: |
|
|
|
|
|
|
|
III. Drug Information (One drug request per form) |
|
|
|
Drug name and strength: |
|
Dosage form: |
Dosage interval (sig): |
Qty per Day: |
|
|
|
|
|
|
|
|
Diagnosis relevant to THIS request: |
|
|
|
|
|
|
|
|
|
|
|
|
Expected length of therapy: |
|
|
|
|
|
|
|
|
|
|
|
|
Medication History for this Diagnosis |
|
|
|
|
|
|
|
|
|
|
|
|
A. Is member currently treated on this medication? |
|
|
|
|
|
yes; How Long?_______________ [go to item B] |
no |
[skip items B & C; go to item D] |
|
|
|
|
|
|
|
|
B. Is this request for continuation of a previous approval? |
|
|
|
|
|
yes |
[go to item C] |
no |
[skip item C; go to item D] |
|
|
|
|
|
|
C. Has strength, dosage, or quantity required per day increased or decreased? |
|
|
|
yes |
[go to item D] |
no |
[skip item D; indicate rationale for continuation in Section IV and submit form] |
|
|
|
|
|
|
|
D. Please indicate previous treatment and outcomes below. |
|
|
|
|
|
Drug Name |
|
|
Dates of Therapy |
|
|
Reason for Discontinuation |
|
(include strength and dosage) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NOTE: Confirmation of use will be made from member history on file; prior use of preferred drugs is a part of the exception criteria. The IlliniCare Health Plan Preferred Drug List (PDL) is available on the IlliniCare Health Plan website at www.illinicare.com .
IV. Rationale for Request / Pertinent Clinical Information (Required for all Prior Authorizations)
Appropriate clinical information to support the request on |
Provider Signature: |
Date: |
the basis of medical necessity must be submitted. |
|
|
|
|
|
US Script will respond via fax or phone within 24 hours of receipt of all necessary information, except during weekends and holidays. Requests for prior authorization (PA) must include member name, ID#, and drug name. Incomplete forms will delay processing. Please include lab reports with requests when appropriate (e.g., Culture and Sensitivity; Hemoglobin A1C; Serum Creatinine; CD4; Hematocrit; WBC, etc.)
*Contact Caremark at 800-237-2767 for Biopharmaceutical Products.