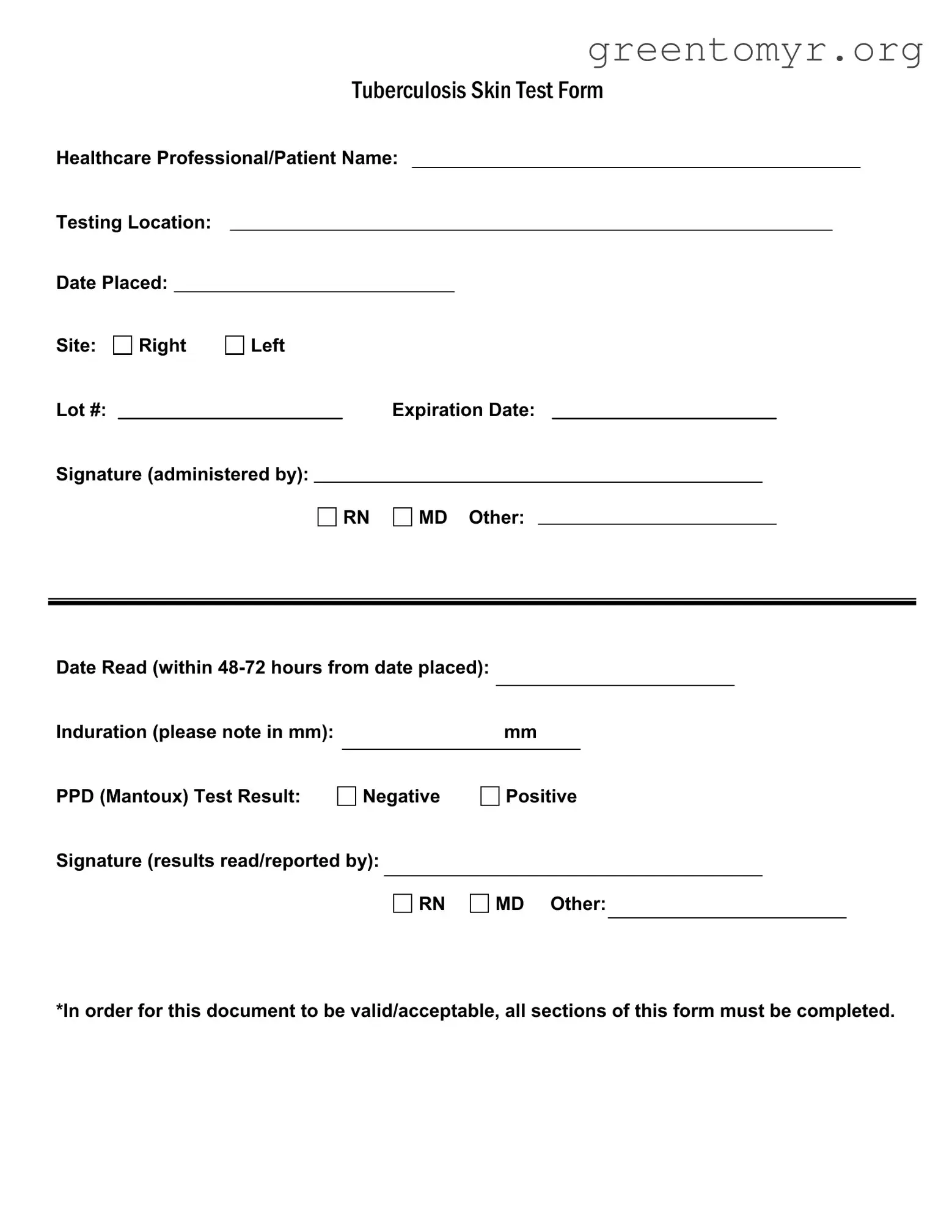
Filling out the Tuberculosis (Tb) Test form may seem straightforward, but it’s crucial to avoid common mistakes. One frequent error occurs in the completion of patient information. Omitting the patient’s name or the testing location can lead to confusion and may delay necessary follow-up actions.
Another mistake involves misrecording dates. It is vital to ensure that both the date placed and the date read are accurately documented. Missing or incorrect dates could compromise the test results and impact subsequent health actions.
Many individuals fail to choose a site for the test, whether the right or left arm, leading to additional complications. It’s essential to clearly indicate where the test has been administered, as this ensures proper record-keeping and future reference.
Lot number and expiration date entries are often overlooked. Without these details, the validity of the test can be questioned. Each section of the form is interconnected, and missing information can render the entire document invalid.
Inaccurate measurement of induration is another vital mistake. The form requires a specific mm measurement, and providing incorrect details may skew the test results. Always double-check this section to ensure accuracy.
Signature errors can also derail the process. Ensure that the individual administering the test and the one reading the results both sign the form. An unsigned test can raise doubts about the authenticity of the results.
It’s not uncommon for people to respond incorrectly to the PPD (Mantoux) Test Result section. Confusing 'negative' with 'positive' can lead to serious misunderstandings regarding a person’s health status.
Lastly, some individuals do not realize the importance of completing all sections of the form. Based on this reminder, incomplete forms may be rejected by healthcare providers. It is crucial to remember that a valid document requires full completion.
Being diligent and aware of these common pitfalls can make a substantial difference. Taking a moment to review the form thoroughly before submission will help in avoiding these mistakes and ensure a smooth testing experience.