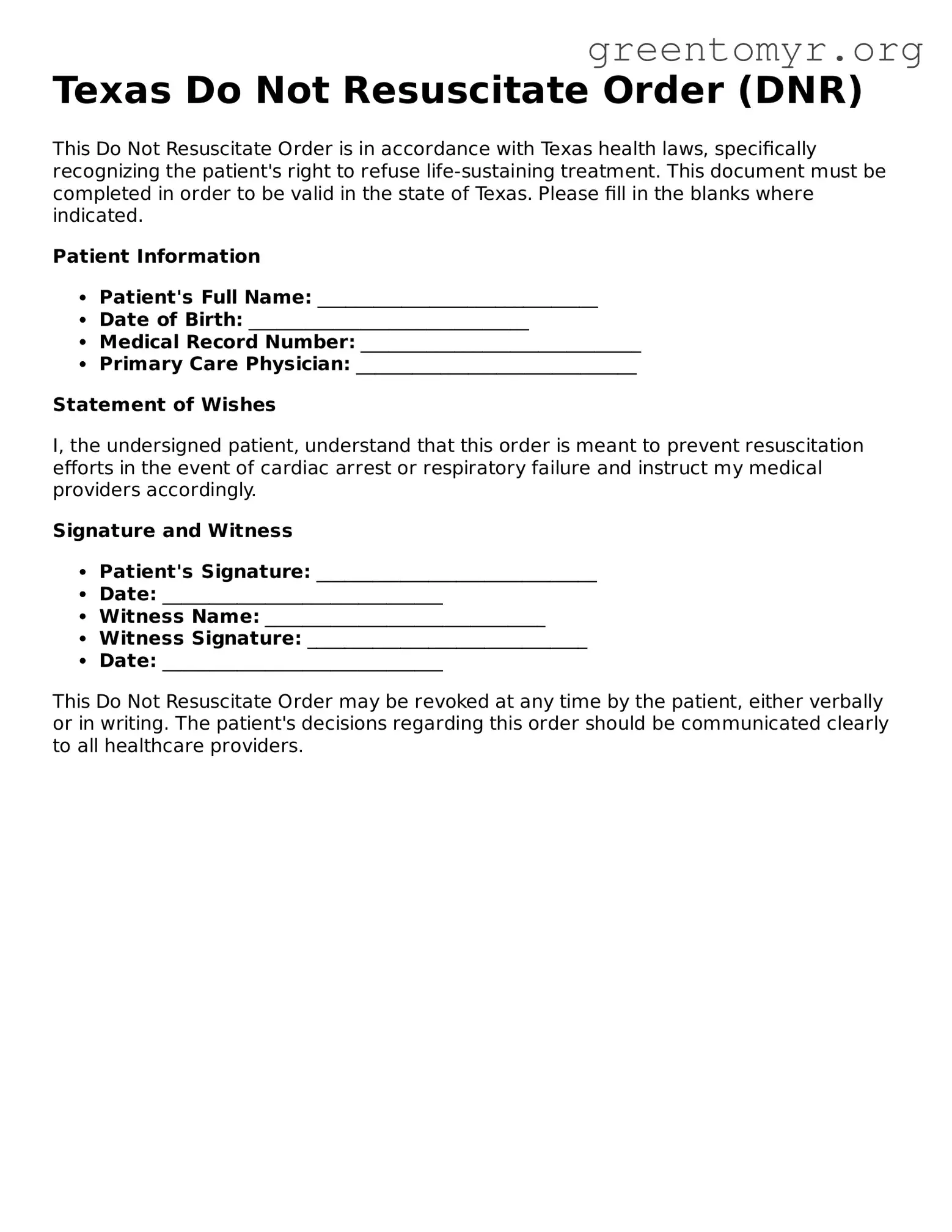
Texas Do Not Resuscitate Order (DNR)
This Do Not Resuscitate Order is in accordance with Texas health laws, specifically recognizing the patient's right to refuse life-sustaining treatment. This document must be completed in order to be valid in the state of Texas. Please fill in the blanks where indicated.
Patient Information
- Patient's Full Name: ______________________________
- Date of Birth: ______________________________
- Medical Record Number: ______________________________
- Primary Care Physician: ______________________________
Statement of Wishes
I, the undersigned patient, understand that this order is meant to prevent resuscitation efforts in the event of cardiac arrest or respiratory failure and instruct my medical providers accordingly.
Signature and Witness
- Patient's Signature: ______________________________
- Date: ______________________________
- Witness Name: ______________________________
- Witness Signature: ______________________________
- Date: ______________________________
This Do Not Resuscitate Order may be revoked at any time by the patient, either verbally or in writing. The patient's decisions regarding this order should be communicated clearly to all healthcare providers.